Since the launch of OpenAI’s GPT-4, the healthcare industry has been experiencing unprecedented change driven by advancements in Artificial Intelligence, particularly generative models. In a podcast episode from Microsoft Research, Peter Lee revisits predictions made in the book ´The AI Revolution in Medicine´ and explores how these technologies are physically impacting real-world healthcare delivery, patient experiences, and medical workforce dynamics. Guests Ethan Mollick, a Wharton School professor, and Azeem Azhar, a renowned tech writer, analyze how Artificial Intelligence is both disrupting and augmenting medical practice and healthcare industry systems.
Ethan Mollick highlights the duality of emotions that come with Artificial Intelligence adoption: excitement about productivity and the emotional challenge when technology encroaches on tasks once thought uniquely human. He notes that while individual clinicians and staff are experiencing notable efficiency gains—like automating encounter notes or reducing administrative burdens—these improvements rarely ripple organically through organizational structures. Instead, systemic inertia, management inefficiencies, and risk aversion often stall the realization of broader benefits. Mollick emphasizes that, unlike past waves of technology, generative Artificial Intelligence´s utility emerges fastest when organizations encourage active internal experimentation rather than waiting for top-down or vendor-driven change.
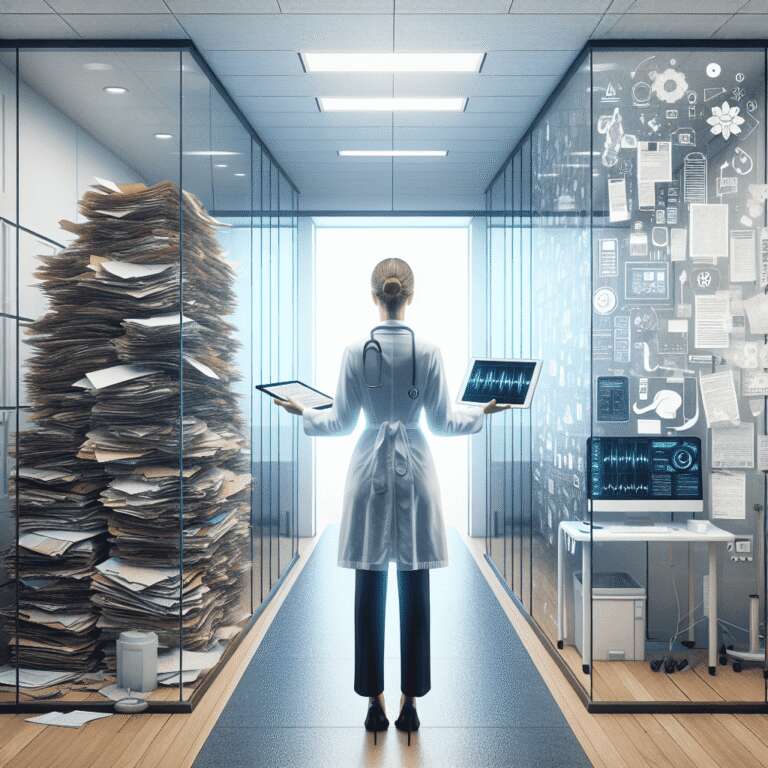
Azeem Azhar, whose expertise spans economics and technology, reflects on the systemic complexity and regulatory nuances of medicine compared to other sectors like finance. He discusses the shift toward consumerization of healthcare, as patients and clinicians increasingly interact with artificial agents for health monitoring, diagnosis, and self-care guidance, citing examples such as medical scribing automation and wearable health tech. Azhar also stresses that medicine’s unique regulatory environment, stakeholder dynamics, and practitioner traditions both slow and structure the adoption of Artificial Intelligence, but inevitable systemic change is underway. The conversation forecasts a future in which clinicians, augmented by Artificial Intelligence, can focus on higher-value interactions while much routine cognitive work is automated, and patients benefit from continuous, personalized health engagement. Both interviewees agree that as Artificial Intelligence becomes more integrated, educational systems, accreditation bodies, and regulatory frameworks must evolve rapidly to keep pace with new capabilities and the shifting definitions of expertise, productivity, and safety in healthcare.
The episode concludes with optimism about Artificial Intelligence’s potential to relieve workforce shortages, reduce burnout, and personalize care, while also acknowledging the daunting challenge of adapting healthcare’s deeply entrenched systems. These discussions underscore that for true transformation, both individual behaviors and organizational structures must evolve, demanding risk-tolerant leadership, cross-disciplinary education, and continuous experimentation with new technologies.